The broken metabolism in Hunter syndrome
Understanding Hunter syndrome, a genetic metabolic disease
The body is a complex system and within it chemical processes occur that generate and break down substances. These chemical reactions work in combination as a process called metabolism, the purpose of which is to maintain normal cell, tissue and organ function. The breakdown of substances occurs within each individual cell in specialised compartments called lysosomes.
Hunter syndrome is a rare genetic, metabolic disease. Affected children are missing, or deficient in, the lysosomal enzyme iduronate-2-sulfatase, or I2S, which is responsible for metabolising specific sugar molecules known as glycosaminoglycans, or GAGs. (To learn more about the genetics of Hunter syndrome please see ‘ The Hunter syndrome gene‘)


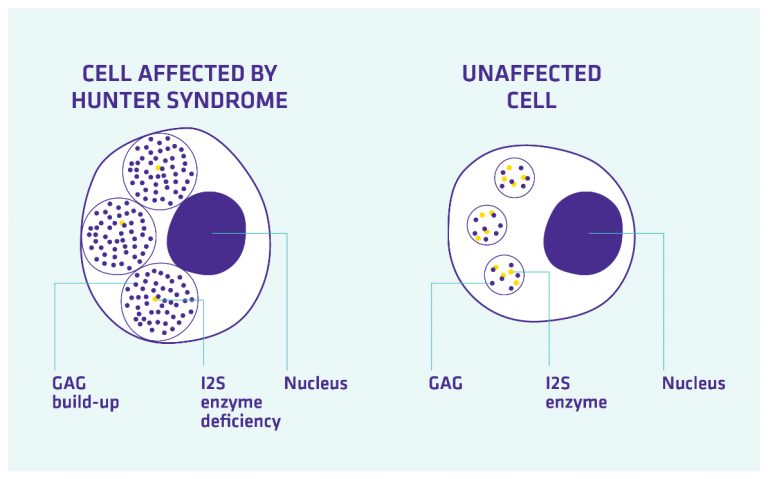
Figure 1: Progressive accumulation of GAGs in cells of children with Hunter syndrome
GAGs are long molecules which are present in all tissues and organs to provide support to cells. GAGs are constantly recycled; being produced and then broken down as required. I2S is able to metabolise two specific types of GAGs known as heparan sulfate and dermatan sulfate.
Dermatan sulfate: this is the major GAG in skin and is also distributed in tendons, ligaments, cartilage and other tissues.
Heparan sulfate: this is associated with supportive tissue in skin, muscle and nervous cells, in addition to the lungs, liver, brain, and aorta in the heart.
In Hunter syndrome GAGs cannot be broken down, but new GAGs continue to be made. This results in the continuous accumulation of GAGs in the lysosomes of cells. These lysosomes begin to swell, affecting cell function which in turn causes multi-organ damage with many widespread symptoms as detailed below.
Clusters of symptoms
Children with Hunter syndrome present with a variety of signs and symptoms, however, these generally occur as a recognisable ‘cluster’ of childhood illnesses with an average symptom onset of 18 months. Common symptoms that may occur early in the disease’s course are:
- Facial features such as prominent brow, broad nose and thick lips
- Recurrent chest infections
- Chronic runny nose
- Upper airway restriction, including noisy breathing and snoring
- Frequent ear infections and subsequent hearing loss
- A distended abdomen (caused by liver or spleen enlargement)
- Umbilical and inguinal hernias
- Frequent or long term diarrhoea
- Joint stiffness, which may lead to restricted movement
- Delays in childhood development (e.g. delayed walking and speech)
Who should I speak to if I’m concerned my child may have Hunter syndrome?
It is crucial to remember that many of these signs and symptoms are common in childhood, but it is the combination of them that may indicate Hunter syndrome. If you think that your child has two or more symptoms of Hunter syndrome, speak to your doctor.

-
Find out more about the signs and symptoms of Hunter syndrome
Take a look around huntersyndrome.info to learn more about the causes, signs and symptoms and real-life stories of families affected by Hunter syndrome, and speak to your doctor if you have any questions.